Treating
Keratoconus
London | Birmingham | Leeds
Speak to our specialists
Latest keratoconus treatment with the team involved in the development of Cross-Linking (CXL) treatment — and first UK clinic to provide it.
London | Birmingham | Leeds
Speak to our specialists
Latest keratoconus treatment with the team involved in the development of Cross-Linking (CXL) treatment — and first UK clinic to provide it.
I flew to London from Canada to do the cross-linking for my keratoconus at Accuvision… Everything about my experience was (and still is) perfect.
They personalised every aspect of my care so that I achieved the best vision possible with my condition. I have been able to achieve 20/20 vision…
I had Corneal Collagen Cross-linking carried out to both eyes and have now achieved the visual standard required for commercial pilots.
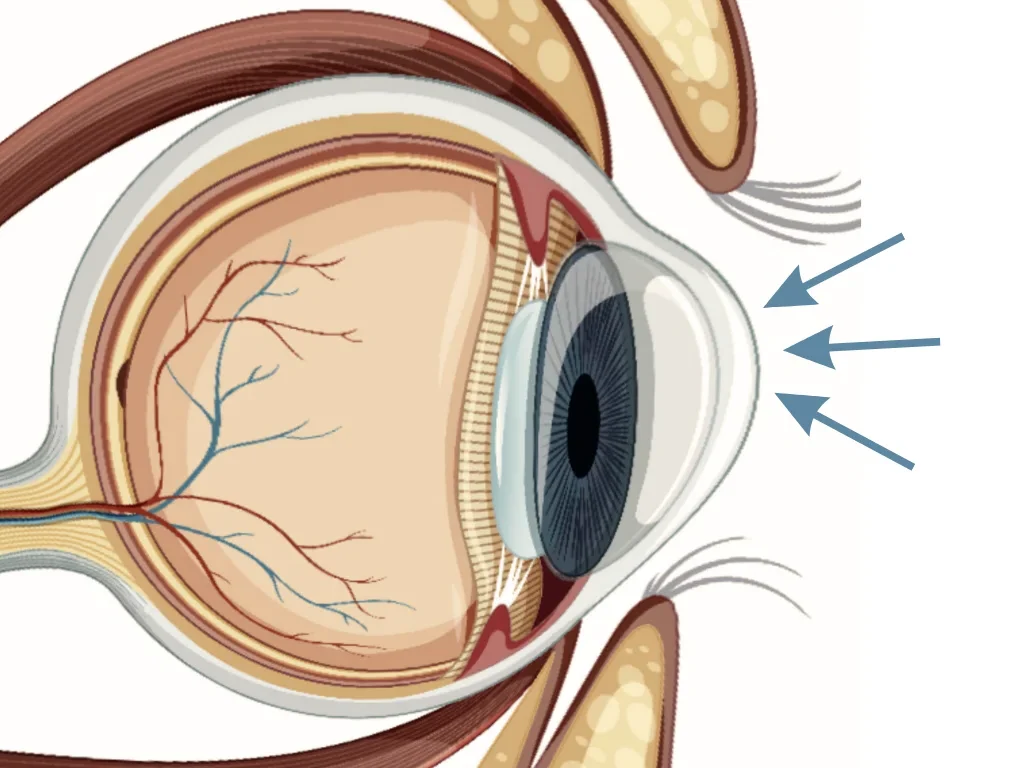
Keratoconus is a condition that weakens and thins the cornea (the transparent window at the front of the eye). This results in a cornea that has a ‘cone-shaped’ forward bulge, leading to myopia (short-sightedness), astigmatism (blurry vision), or severe vision loss if left untreated.
Keratoconus can come in various forms and severity levels, but some common symptoms include:
Parents with Keratoconus should ensure their children’s eyes are examined from the age of 10 at a specialised clinic equipped to detect the condition early.
Intense, repeated eye-rubbing can cause keratoconus — especially when using the back of the knuckle. This is the #1 most dangerous, avoidable risk factor for Keratoconus.
Keratoconus usually starts in teenage years — but can show up in childhood or later on in adulthood.
People with hay fever or atopic conditions, like eczema, are more prone to eye-rubbing.
Makes your eyes feel dryer and leads to more eye-rubbing. Smoking can also cause meibomian gland dysfunction, drying out your eyes and causing more friction.
Dry or windy environments, or poorly fitting contact lenses, can make your eyes dryer and result in more eye-rubbing.
Collagen disorders include Ehlers-Danlos Syndrome (EDS), Marfan Syndrome and Ostogenesis Imperfecta.
According to a study in the European Journal of Human Genetics, some of the genes involved in these disorders play a role in Keratoconus.
A study published in Frontiers of Medicine showed that lower testosterone levels in both male and female Keratoconus patients and higher estradiol levels in male Keratoconus patients may contribute to corneal thinning and steepening — which are characteristic of KC.
Certain disorders like diabetes, Down syndrome, and sleep apnea make keratoconus more likely.
Well-fitted lenses can help with maximising vision, but can’t treat keratoconus as they don’t stop the progression of the condition.
Intacs are a surgical procedure effective for mild to moderate keratoconus. When they are inserted into the eye, they reshape the cornea by flattening it closer to its original shape.
Monitoring your vision closely and being attentive to any vision changes or new symptoms is crucial so that we can promptly address any new issues.

Living with keratoconus? These self-care tips will help you maintain your corneal health and keep your vision sharp. Let’s dive in!
Including any medications, eye drops, special contact lenses, and follow-up appointments. Consistency is key here.
Wear sunglasses with 100% UV protection. This is especially important after procedures like corneal cross-linking (CXL).
We know it can be tempting, but try to resist rubbing your eyes. This can exacerbate corneal changes. If you're experiencing dry eyes, use the prescribed artificial tears.
Use the recommended eyelid cleansers and follow proper hygiene practices, especially if you wear contact lenses. This helps prevent infections.
Hydration supports overall eye health. It can help alleviate some of the dry eye symptoms common in keratoconus patients.
If you have allergies, it's important to keep them under control. We can discuss strategies that won't interfere with your keratoconus management.
A balanced diet rich in vitamins A, C, E, and omega-3 fatty acids can support your overall eye health. Consider incorporating foods like leafy greens, fish, and citrus fruits.
If you experience any sudden changes in vision, increased pain, or signs of infection, please seek immediate care. Early intervention can be crucial.
Remember, managing keratoconus is a collaborative effort. By following these self-care practices, you can preserve your vision and eye health.
If you have any questions about these tips or your treatment, please don’t hesitate to give us a call.

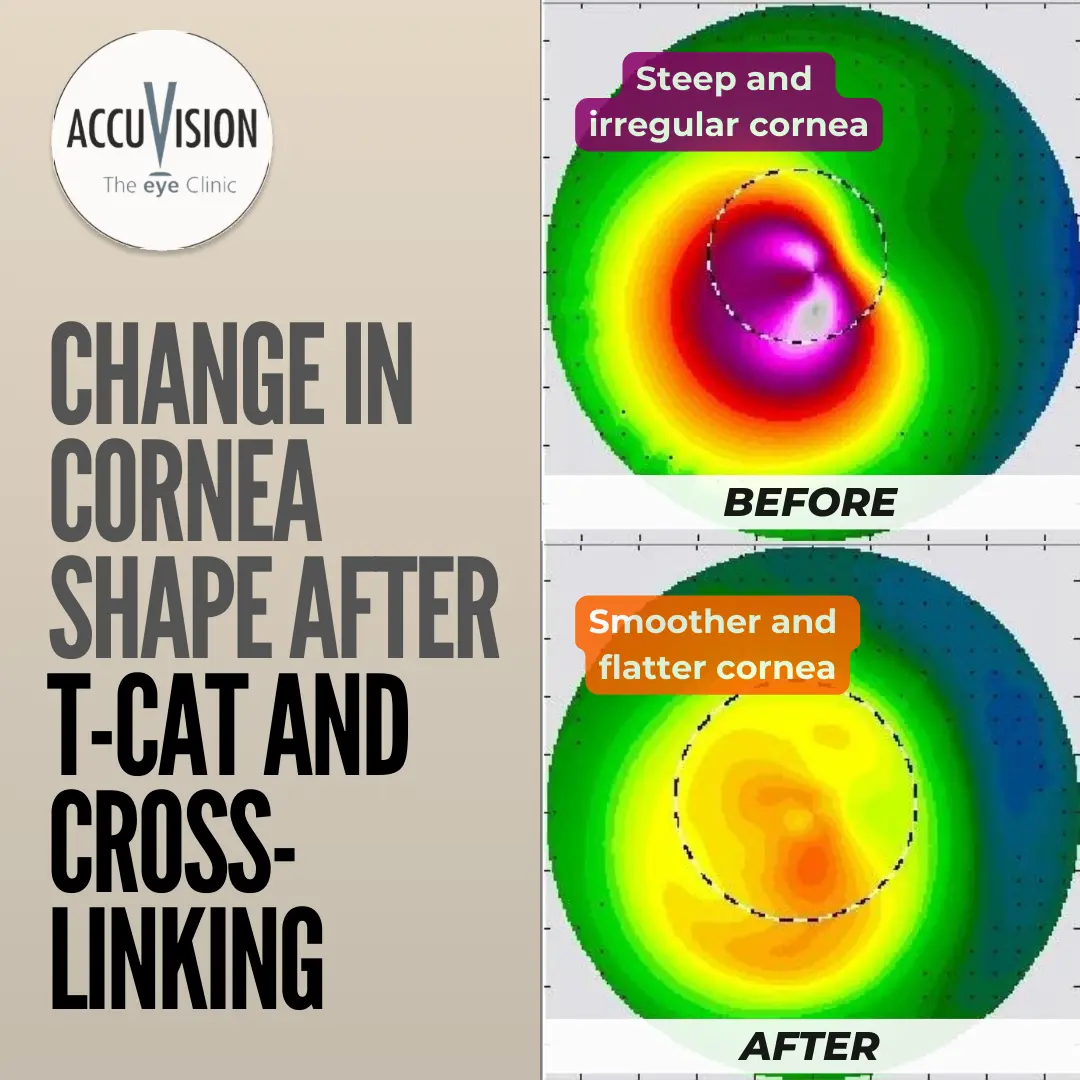
We use advanced diagnostics to map even extremely distorted corneas with perfect precision.
We use this diagnostic data to plan a customised Laser treatment to normalise corneal irregularities.
Many Keratoconus patients experience a substantial improvement in their vision after the T-CAT Laser treatment.
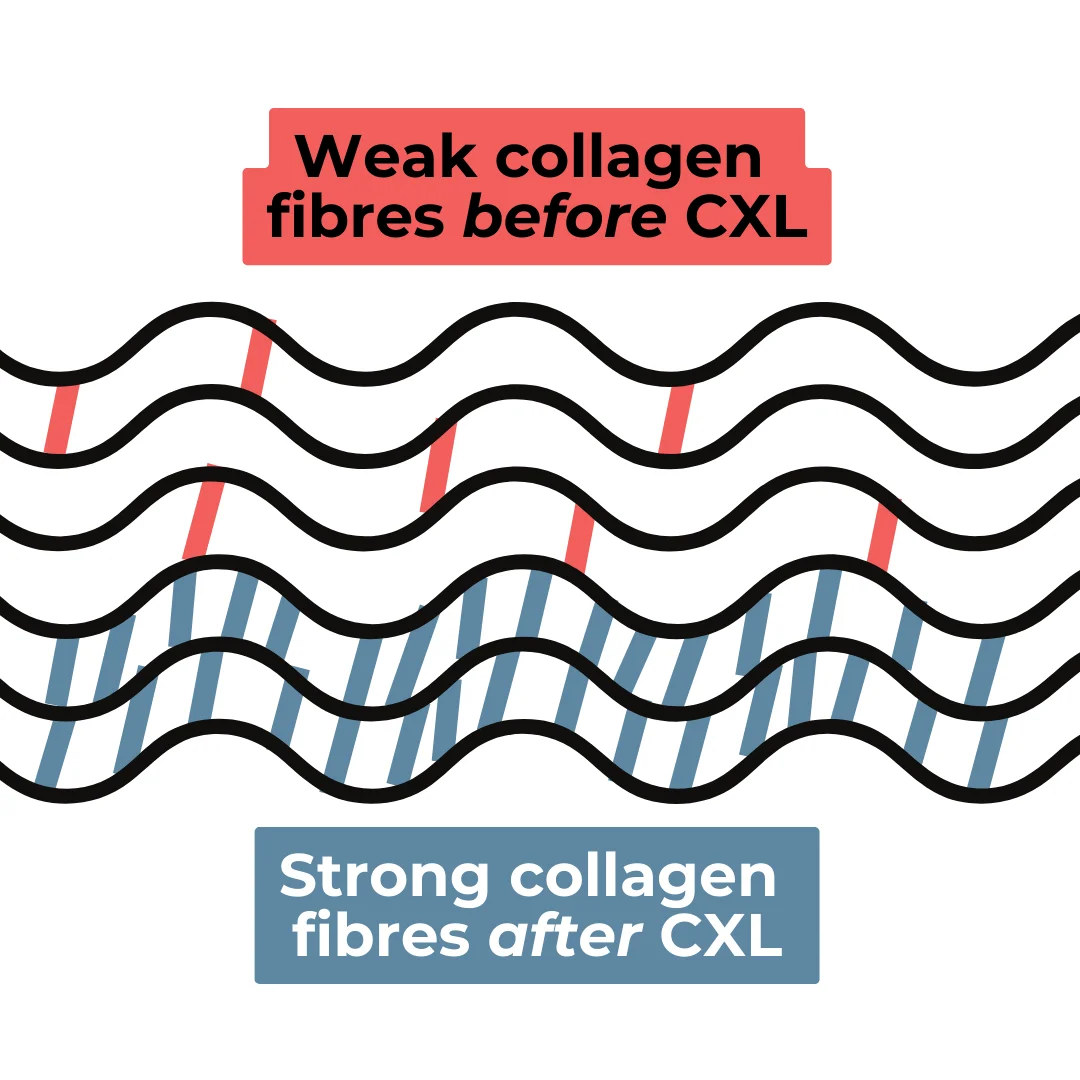
Finally, we apply CXL treatment to strengthen the cornea for lasting vision quality.
Diagnosed at 19, Charlene spent 9 years with ineffective rigid gas permeable lenses, frequent prescription changes and eye irritation until she found AccuVision:
“I describe this as previously looking through black and white television to now seeing things in high definition. This has been life changing for me, my family, and friends.”
She had lost hope due to unsuccessful treatments in the past:
“I had issues in the past with previous optometrists struggling to find RGPS to fit…. However, to my surprise… I managed to see out of my right eye for the first time in years. I was very emotional and it was almost a miracle that they had accomplished this.”
Our advanced screening, prompt diagnosis and holistic Keratoconus treatment provide life-changing outcomes for our patients, including:
All patients exhibited a reduction in irregular astigmatism
Most patients showed improved glasses prescription and Best Corrected Visual Acuity (BCVA).
Average improvement in topographical asymmetry was 7.8D. This meant reduced corneal distortion and improved profile.
Majority of patients stopped keratoconus progression.
No patients lost Best Corrected Visual Acuity
Patient | Difference along steepest meridian: | Gain/Loss BCVA (Snellen Lines) | ||
Pre-Op | Post-Op | Improvement | ||
SMR | 8D | 2.5D | 5.5D | 1 |
SML | 13D | 3D | 10D | = |
MGR | 15D | 2D | 13D | 3 |
GCR | 3D | 1.5D | 1.5D | +1/2 |
GCL | 8.5D | 0.5D | 8D | 1 |
SBR | 5D | 3D | 2D | = |
SBL | 8D | 3.5D | 4.5D | 1 |
PBR | 7D | 5D | 2D | = |
PBL | 13D | 7D | 6D | 2 |
IOR | 18D | 4D | 14D | 1 |
IOL | 21D | 11D | 10D | +1/2 |
PJR | 18D | 4D | 14D | 4 |
PJL | 10D | 2D | 8D | 1 |
JOR | 17D | 6D | 11D | = |
JOL | 14.5D | 2.5D | 12D | = |
MWR | 11D | 6D | 5D | 1 |
LSR | 6D | 2D | 4D | = |
PPR | 9D | 0D | 9D | 1 |
PPL | 7D | 3D | 4D | = |
Keratoconus cannot be completely cured, but its progression can be halted or slowed down through specialised treatments. These treatments aim to improve vision and stabilize the cornea.
The choice of treatment depends on the severity of the condition and individual factors. Regular monitoring and early intervention are crucial to managing keratoconus effectively.
Yes, many individuals with keratoconus can lead normal lives with proper management and treatment.
While it may require ongoing eye care and the use of corrective lenses or other interventions, most people with keratoconus can maintain their daily activities, including work, education, and recreational pursuits.
Regular check-ups with an eye care specialist are essential to monitor the condition and make necessary adjustments to treatment.
Keratoconus is a progressive eye condition, and its seriousness can vary from person to person.
In its early stages, it may cause mild visual disturbances that can be managed with glasses or soft contact lenses.
However, in advanced cases, when the cornea becomes severely distorted, it can lead to significant vision impairment.
While keratoconus is not life-threatening, its impact on quality of life underscores the importance of early diagnosis and appropriate treatment.
Two common signs of keratoconus include:
Other signs may include frequent changes in prescription eyeglasses or contact lenses, ghosting or multiple images, and eye irritation.
Keratoconus is typically managed rather than “fixed” in the traditional sense. The best chance
The choice of treatment depends on the individual’s specific condition and its severity. Early diagnosis and regular monitoring by an eye care specialist are crucial to determine the most appropriate treatment plan for each person with keratoconus.
While it’s possible to wear glasses for keratoconus, their effectiveness can be limited. Even after stabilizing the corneal surface as much as possible, it remains relatively irregular compared to a “normal” eye. This irregularity can compromise visual acuity, making customised contact lenses a preferable option for clearer vision.
Choosing the right vision correction method depends on individual factors and the extent of corneal irregularity. Your eye care specialist can recommend the best option based on your specific needs and condition.
Soft contact lenses moulds to the shape of the cornea, which, if very distorted from Keratoconus, can mean limited improvement in vision.
In contrast, rigid or scleral lenses lenses are customised to fit to the unique shape of each cornea. They effectively “mask” the corneal distortion, resulting in improved vision quality.
After CXL treatment, the corneal surface is much more regular and therefore more responsive to a lens. Once the lens-fit is improved, vision is enhanced and lenses become more comfortable.
Additionally, the Accuvision Team is highly experienced and specialised in customised contact lens fits. This is how many of our patients achieve comfortable vision quality, even if they’ve struggled with lenses previously.
Achieve clear vision under the personalised guidance of our clinicians. Simply fill this form and we will be in touch to answer all of your questions. Schedule your consultation now — proceed with informed confidence: