Keratoconus Treatment- Types, Symptoms and Treatments

Jump To Section
What is Keratoconus | Causes | Types | Underlying Biology | Symptoms | Treatments | Self-Care | Keratoconus Treatment in 2023 | CXL Treatment at AccuVision | T-CAT Treatment At AccuVision | Intacs at AccuVision | FAQ
What is Keratoconus?
Keratoconus is a condition that affects the cornea (the transparent window at the front of the eye). Keratoconus causes changes within the structure of the cornea making it weaken and thin resulting in a 'cone-shaped' forward bulge. It can lead to myopia (short sightedness) and, if the steepening is uneven, also astigmatism (distortion of vision). With keratoconus, visual distortion can become difficult to correct with spectacles, although contact lenses can provide more functional visual performance.What Causes Keratoconus?
Keratoconus is a complex eye disorder that manifests in various forms and severity levels. Its symptoms can lead to erratic shifts in vision and eye function, often causing considerable discomfort and disruptions in daily life.-
Family History
Parents with keratoconus should get their children’s eyes checked for signs from 10 years of age. -
Eye-Rubbing Habit
Intense, repeated eye-rubbing, especially when using the back of the knuckle, causes trauma to the cornea over time. It aggravates the condition and makes keratoconus progress faster. -
Smoking
Smoke exposure results in dryness and increases the likelihood of eye-rubbing. Moreover, meibomian gland dysfunction and dryness due to smoke can increase friction during eye-rubbing episodes. -
Age Range
Keratoconus usually starts in teenage years but can show up earlier in childhood or later into adulthood. -
Environmental Factors
External elements, such as chronic eye rubbing due to dry or windy environments, or poor fitting contact lenses, can contribute to the progression of keratoconus. -
Collagen Abnormalities
Collagen is a vital protein in the cornea that provides structural support. Anomalies in collagen composition or cross-linking may weaken the cornea, making it susceptible to bulging and deformation. Such collagen disorders include Ehlers-Danlos Syndrome (EDS), Marfan Syndrome and Ostogenesis Imperfecta. -
Hormonal and Biochemical Changes
Some studies suggest that hormonal imbalances or changes during puberty may influence the development of keratoconus. Enzyme activity in the cornea might also be altered in individuals with the condition. -
Chronic Inflammation
Some researchers believe that inflammatory responses within the cornea could play a role in the development of keratoconus. Chronic inflammation might lead to structural changes in the cornea. -
Certain Disorders
Certain disorders like diabetes, Down syndrome, and sleep apnea make the incidence of keratoconus more likely. -
Eye Allergies and Atopic Conditions
Individuals with allergies like hay fever, or atopic conditions (e.g., eczema) may be more prone to eye rubbing and, consequently, keratoconus.
Types of Keratoconus
Keratoconus is a complex eye condition that can manifest in several ways, each with its own characteristics and severity. Understanding the different types of keratoconus is crucial for diagnosis and appropriate management.-
Incipient Keratoconus
Incipient keratoconus refers to the earliest stage of the condition, often characterised by minor changes in corneal shape. Patients with incipient keratoconus may experience mild visual disturbances and astigmatism. Early detection and intervention are vital to prevent progression. -
Nipple Cone (Nipple-like Apex) Keratoconus
This type of keratoconus is named for its characteristic conical protrusion, which resembles a nipple. Nipple Cone keratoconus can lead to significant visual distortion and difficulty with contact lens fitting. -
Oval Cone (Oval-shaped) Keratoconus
In Oval Cone keratoconus, the cornea takes on an oval or egg-like shape. This variation often results in irregular astigmatism and challenges in achieving optimal visual correction. -
Segmented (Fragmented) Keratoconus
Segmented keratoconus is marked by localised areas of corneal thinning, creating a fragmented appearance. Visual symptoms can vary depending on the extent and location of the segments. -
Advanced (Severe) Keratoconus
Advanced keratoconus represents the most progressed form of the condition. The cornea exhibits significant thinning, steepening, and irregularity, causing substantial visual impairment. Optimal treatment options for advanced keratoconus may include corneal transplantation. -
Bilateral Keratoconus
Bilateral keratoconus affects both eyes and is more common than unilateral cases. It can vary in severity between the two eyes, making precise management crucial. -
Unilateral Keratoconus
Unilateral keratoconus is relatively rare and affects only one eye. It may present unique challenges in diagnosis and treatment, as the unaffected eye can compensate for visual deficits. -
Pellucid Marginal Degeneration (PMD)
While technically distinct from keratoconus, PMD shares similar corneal thinning and steepening characteristics. PMD typically affects the inferior cornea, causing irregular astigmatism.
Understanding the Biology of Keratoconus
Keratoconus is a complex eye disorder characterised by structural changes in the cornea, the clear front surface of the eye responsible for focusing light onto the retina. This condition involves several underlying biological factors. One key factor is the irregular arrangement of collagen fibres within the cornea. Collagen, a crucial protein, provides strength and structure to the cornea. In keratoconus, these collagen irregularities weaken the cornea, leading to its progressive bulging and the characteristic conical shape.What Are the Signs and Symptoms of Keratoconus?
Recognising the signs and symptoms of keratoconus is vital for early diagnosis and effective treatment. While the condition can manifest differently in individuals, some common indications include:- Blurred and Distorted Vision: One of the earliest signs of keratoconus is a gradual decline in vision quality. Individuals may notice that their vision becomes increasingly blurred and distorted, making it challenging to read, drive, or perform daily tasks.
- Frequent Changes in Eyeglass or Contact Lens Prescription: As the cornea's shape changes, individuals with keratoconus often require frequent updates to their eyeglass or contact lens prescriptions. These individuals may also have high or advancing astigmatism and often find that standard vision correction becomes less effective over time.
- Increased Sensitivity to Light (Photophobia): Many people with keratoconus experience heightened sensitivity to light (photophobia), which can cause discomfort and excessive squinting, particularly in bright environments.
- Halos and Glare: When looking at light sources, such as car headlights at night, individuals with keratoconus may see halos or glare around the lights, further compromising their vision quality.
- Double Vision (Ghosting): Double vision, or ghosting, can occur when the distorted cornea causes light to scatter irregularly within the eye, creating multiple images of a single object.
- Frequent Eye Rubbing: Constant eye rubbing, often due to irritation or discomfort caused by keratoconus, can exacerbate the condition and lead to increased corneal thinning.
- Corneal Changes: In advanced cases, an eye care professional may observe physical changes in the cornea, such as thinning, scarring, or the development of pronounced cone-shaped bulges during a comprehensive eye examination.
How is Keratoconus Treated?
There is no "keratoconus cure", therefore, treatments for keratoconus are aimed at optical improvement. Depending on the degree of corneal bulging, thinning of the cornea, and resultant astigmatism, a number of options can be considered:Contact Lenses
In advancing cases, contact lenses (rigid/hard lenses) can help to improve keratoconus vision, yet they cannot stop the progression of the condition.Corneal Ring Segments Insert (Intacs)
Corneal Transplantation
Up until a few years ago, the only therapeutic option for vision restoration in advanced cases of keratoconus was corneal transplantation (penetrating keratoplasty) to achieve better vision.Corneal Collagen Cross-Linking
An established and proven treatment called Corneal Collagen Cross-linking with Riboflavin (C3-R®) is now available for keratoconus. This minimally invasive procedure uses a combination of Riboflavin drops and ultra-violet light that reacts with the tissues in the cornea, strengthening them by creating more 'cross-linking' among them. The resulting increased stiffness and rigidity of the cornea stabilises ectasia.Self Care After Keratoconus Treatment
Receiving treatment for keratoconus is an essential step in managing the condition and preserving your visual function. But it's crucial to follow certain self-care practices to support your recovery and maintain the best possible eye health.- Follow Your Doctor's Instructions: This may include using prescribed medications, eye drops, or wearing special contact lenses. Make sure to attend all follow-up appointments as scheduled.
- Protect Your Eyes from UV Exposure: UV rays can be harmful to your eyes, especially after treatments like Corneal Collagen Cross-Linking (C3-R®). Wear sunglasses that provide UV protection when outdoors to shield your eyes from potential harm.
- Avoid Eye Rubbing: Post-treatment, it's vital to refrain from rubbing your eyes. Excessive eye rubbing can irritate the cornea and disrupt the healing process. If your eyes itch, use artificial tears or consult your doctor for appropriate solutions.
- Maintain Good Eye Hygiene: Keep your eyes clean and free from debris. Use a mild, preservative-free eyelid cleanser to gently clean the eyelid margins. Maintaining good hygiene reduces the risk of infection.
- Stay Hydrated: Drink an adequate amount of water to ensure your body and eyes stay hydrated. Proper hydration can help prevent dry eyes, which can be a concern after some keratoconus treatments.
- Monitor Your Vision: Pay close attention to any changes in your vision or the appearance of new symptoms. If you notice any unusual issues, contact your eye specialist promptly.
- Manage Allergies: If you have allergies, managing them effectively can minimise eye irritation and discomfort. Consult with your doctor for suitable allergy management strategies.
- Protect Your Eyes During Sports: If you enjoy sports or physical activities, consider wearing protective eyewear, especially if you've had corneal procedures. This precaution can prevent accidental eye injury.
- Maintain a Healthy Lifestyle: Eating a balanced diet rich in eye-friendly nutrients and maintaining an overall healthy lifestyle can contribute to your eye health. Consider incorporating foods high in vitamins A, C, and E, as well as omega-3 fatty acids.
- Seek Prompt Assistance: If you experience any concerning symptoms such as pain, sudden vision changes, or signs of infection, don't hesitate to contact your eye specialist immediately.
Keratoconus Treatment in 2023
In 2023, significant advancements have been made in the diagnosis and treatment of keratoconus. Let’s take a look at the latest treatments in 2023 for keratoconus:- Early Detection and Diagnosis: With the advent of advanced imaging technologies such as corneal topography and optical coherence tomography (OCT), ophthalmologists can now detect and diagnose keratoconus at an early stage.
- Customised Treatment Approaches: The treatment of keratoconus has become more personalised, taking into account the unique characteristics of each patient’s cornea. This includes the use of specialised contact lenses, such as scleral lenses, hybrid lenses, and custom soft lenses, to improve visual acuity and comfort.
- Corneal Cross-Linking (CXL): Corneal cross-linking is a minimally invasive procedure that involves the application of riboflavin (vitamin B2) eye drops followed by exposure to ultraviolet (UV) light. This proven treatment for keratoconus helps to strengthen the cornea and, in many cases, serves as a keratoconus permanent treatment.
- Intraocular Collagen Implants: In recent years, researchers have been refining the use of collagen implants to treat keratoconus. These implants are designed to reinforce the cornea and improve its structural integrity.
- Gene Therapy: Although still in the experimental stage, gene therapy holds promise for the treatment of keratoconus. By targeting specific genes associated with the development of keratoconus, researchers aim to develop gene-based therapies that can potentially prevent or reverse the progression of the disease.
Think you have keratoconus? Here's how AccuVision can help.
Corneal Collagen Cross-Linking (CXL) At AccuVision
How does CXL for Keratoconus work?
Benefits of CXL for Keratoconus
CXL for keratoconus seems effective in stabilising progressive ectasia, and in some patients the treatment gives an additional small measure of benefit in the reduction of corneal steepness and irregularity. This in turn means some reduction in the myopia and astigmatism associated with the ectasia. In the past it was always considered that excimer Laser Eye Surgery correction of myopia or astigmatism was not possible when ectasia was present. This was because by removing corneal tissue with the laser the cornea would become even less stable and the ectasia would be made worse. However, once the keratoconus condition is stabilised by CXL it may be possible to perform limited amounts of Laser Eye Surgery whilst still maintaining structural stability of the cornea. Such Laser Eye Surgery treatment would usually be aimed at restoring a more spherical shape to the cornea (custom ablation). Any remaining optical defect could then potentially be corrected by spectacles, or alternatively with soft contact lenses, or by phakic intra-ocular lens implants.How is Keratoconus CXL Treatment Given?
The bulk of the cornea is made from collagen fibres which are arranged in bundles. The strength and rigidity of the cornea is partly determined by how strongly the fibres are linked together. Over the course of a lifetime the cornea becomes progressively stiffer due to natural cross-linking between the fibres. Riboflavin (vitamin B2) is a naturally occurring compound which strongly absorbs UV light. By applying riboflavin to the cornea at the same time as exposing it to a UV light source, the riboflavin not only enhances the cross-linking effect of the UV light, but also absorbs the light to an extent that the inner layers of the cornea and intra-ocular structures are protected from the potentially damaging effects of the light rays.Potential Risks of CXL Treatment for Keratoconus
Keratoconus can be treated with a relatively new procedure called Corneal Collagen Cross-linking with Riboflavin. This is a tried and tested treatment that increases the stiffness and rigidity of the cornea and stabilises ectasia. Patients who previously had progressive ectasia have now been treated and followed for up to five years without evidence of any further change in their condition. At present it is not known whether the stabilising effect of C3-R® on keratoconus is permanent, but the C3-R® treatment could potentially be repeated if it was necessary.Risks of CXL for Keratoconus
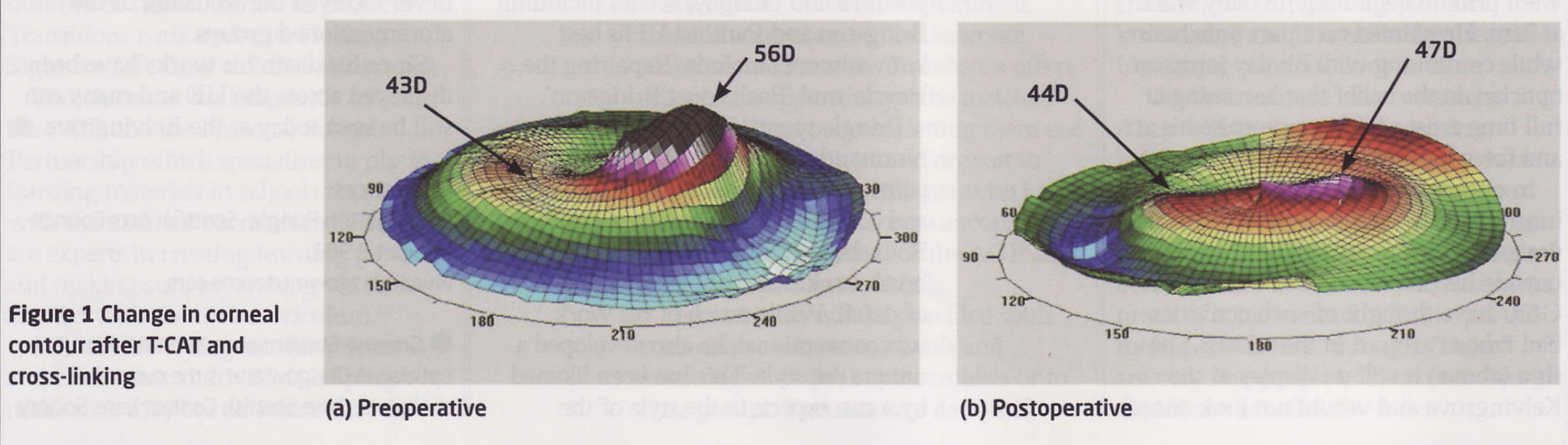
 Topography-Guided Custom Ablation Treatment for Keratoconus (T-CAT)
Topography-Guided Custom Ablation Treatment for Keratoconus (T-CAT)
 T-CAT combined with CXL for Keratoconus
T-CAT combined with CXL for Keratoconus
- Stabilise the cornea.
- Reduce corneal distortion and improve profile.
- Lead to a substantial improvements in eyeglass prescription.
Intacs for Keratoconus
An alternative treatment for keratoconus is the use of Intacs, implanted into the cornea. Intacs are a new surgical treatment for mild to moderate keratoconus. When inserted into the cornea, the Intacs segments make the central corneal profile flatter and more regular, and this reduces the optical defect.Intacs for keratoconus are 'C' shaped segments of perspex (polymethyl-methacrylate or PMMA), that are inserted deep into the corneal stroma. They were originally designed for treatment of low myopia, and typically correct two or three dioptres of myopia or myopic astigmatism. Patients with keratoconus often have moderate or high degrees of myopia and astigmatism due to irregular steepening of the cornea caused by the condition. For these patients, Intacs for keratoconus will reduce the optical defect in the eye and the remaining myopia and astigmatism can then be corrected either with glasses, or by insertion of an Implantable Collamer Lenses (ICL), or by Artisan lens surgery.Intacs for Keratoconus - Surgical Procedure
Insertion of Intacs can be carried out with topical, local, or general anaesthesia according to the patient's preference.- A two millimetre incision is made into the cornea to a depth of about two thirds of its thickness, and a special instrument is then used to prepare the bed into which the Intacs for keratoconus are inserted.
- Once they have been put into position, a single stitch is used to close the small corneal wound.
- Eye drops are used for a few weeks to settle the eye down, but the patient can resume normal activities more or less straight away.
- The corneal suture is removed after a couple of weeks with application of anaesthetic eye drops.